
www.drbriandickinson.com
The Brian Dickinson M.D. Breast Reconstruction Blog is an online professional journal with reflections, comments, experiences, opinions, articles, and patient educational material. Brian P. Dickinson M.D. Inc.


The CT-angiogram has shown great utility for DIEP flap, SIEA flap, free TRAM flap, as well as the pedicle TRAM flap in identifying blood supply to the abdominal tissue used in breast reconstruction.

I have found the CT-angiogram to be very helpful for flap planning in breast reconstruction. The CT-angiogram allows the operative surgeon to have a road map for vessel selection, may facilitate orientation of the flap for breast reconstruction, as well as facilitate positioning of the scar on the abdominal wall for flap harvest.
The CT-angiogram is specifically helpful in the patient who has had previous abdominal operations to determine the integrity of vessels as well as determine which flap may be an appropriate option for the patient such as TRAM, TRAM flap with pre-delay procedure, free TRAM, DIEP, or SIEA.
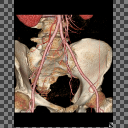
The 3D reconstruction shown below gives an example of how the surgeon can appropriately evaluate vessel integrity in a previously operated abdomen.
Brian P. Dickinson, M.D.


 Proper nutrition should be an important part of everyone's daily life. Both aesthetic and reconstructive surgery place an increased metabolic demand on the body. It is important both pre-operatively and post-operatively to ensure adequate protein intake before and after surgery. Frequently nutrition comes up in consultations, so I have included below a standard post-operative diet protocol as well as an easy method for patients to understand the amount of protein they will need post operatively.
Proper nutrition should be an important part of everyone's daily life. Both aesthetic and reconstructive surgery place an increased metabolic demand on the body. It is important both pre-operatively and post-operatively to ensure adequate protein intake before and after surgery. Frequently nutrition comes up in consultations, so I have included below a standard post-operative diet protocol as well as an easy method for patients to understand the amount of protein they will need post operatively.